A Simple Solution
By ANDREA GERLIN Sunday, Oct. 08, 2006
STRONG MEDICINE: A nurse at the ICDDR hospital in Dhaka treats Rana, a 17-month-old girl suffering from diarrhea and malnutrition, as the child's mother holds her. Diarrhea is the cause of one-third of child deaths in Bangladesh
Most of the tiny patients confined to the children's ward at the International Centre for Diarrhoeal Disease Research (ICDDR) in Dhaka, Bangladesh, are weak, malnourished and dehydrated. They've suffered attack after attack of diarrhea and, in some cases, are clinging to life. Five-month-old Sohag, who is lying on green plastic sheeting in a bed four times her size, had suffered[an error occurred while processing this directive] diarrhea for seven days before she was admitted. Her weight had dropped to 2.75 kg, just over one-third of that expected for her age, and she now seems to be little more than a distended stomach, bulging head and collection of scrawny limbs. According to the chart at the foot of her bed, she may also have pneumonia and sepsis. But at the root of her problem is chronic diarrhea, a daily killer of 5,000 young children in the developing world and the cause of one-third of child deaths in Bangladesh. Her 15-year-old mother, Jharana, had never heard of diarrhea before she was advised to take Sohag to ICDDR's hospital. There, the baby received saline solution through a vein in her arm, and a rice-based solution through a tube in her nose.
By ANDREA GERLIN Sunday, Oct. 08, 2006
STRONG MEDICINE: A nurse at the ICDDR hospital in Dhaka treats Rana, a 17-month-old girl suffering from diarrhea and malnutrition, as the child's mother holds her. Diarrhea is the cause of one-third of child deaths in Bangladesh
Most of the tiny patients confined to the children's ward at the International Centre for Diarrhoeal Disease Research (ICDDR) in Dhaka, Bangladesh, are weak, malnourished and dehydrated. They've suffered attack after attack of diarrhea and, in some cases, are clinging to life. Five-month-old Sohag, who is lying on green plastic sheeting in a bed four times her size, had suffered[an error occurred while processing this directive] diarrhea for seven days before she was admitted. Her weight had dropped to 2.75 kg, just over one-third of that expected for her age, and she now seems to be little more than a distended stomach, bulging head and collection of scrawny limbs. According to the chart at the foot of her bed, she may also have pneumonia and sepsis. But at the root of her problem is chronic diarrhea, a daily killer of 5,000 young children in the developing world and the cause of one-third of child deaths in Bangladesh. Her 15-year-old mother, Jharana, had never heard of diarrhea before she was advised to take Sohag to ICDDR's hospital. There, the baby received saline solution through a vein in her arm, and a rice-based solution through a tube in her nose.
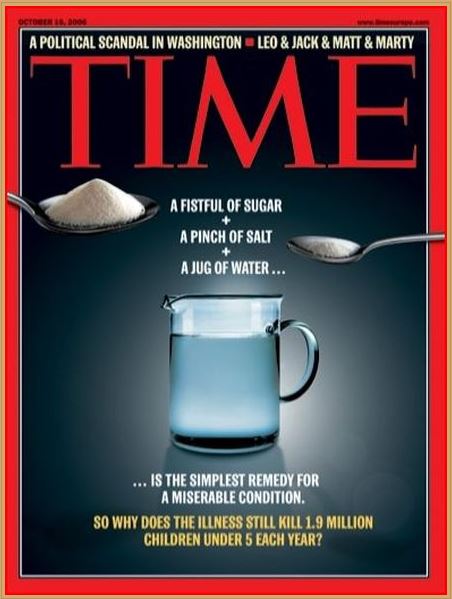
Weak as she is, patients like Sohag who make it to a hospital are the lucky ones. Most of them are treated and released within a few days, as her doctor expected Sohag would be. But many children never reach a treatment center and die from dehydration as they lose critical body fluids faster than they can be replaced. Like Jharana, their family members don't know how to prepare a life-saving remedy that can be assembled for just a few pennies: a large pinch of salt and a fistful of sugar dissolved in a jug of clean water, the simplest recipe for oral rehydration solution. "To save the life of a person with diarrhea is probably the cheapest health intervention you can think of," says David Sack, an American doctor who is the ICDDR's executive director.
Cheap; but nothing like as commonly available as it should be. Oral rehydration has saved the lives of more than 40 million children since it was first put to the test during a cholera outbreak among refugees on India's border with Bangladesh in 1971. But decades later, it remains grossly underused. The result, according to the World Health Organization (WHO): 3 million people a year still die from diarrheal complications, including 1.9 million children under 5, or 17% of the estimated 11 million deaths in that age group. These deaths are largely preventable and unnecessary. "We have the tools to really reduce deaths," says Olivier Fontaine, a diarrheal disease expert at the WHO in Geneva, Switzerland. "The cost of this intervention is minimal. Yet we can't get it to every child that needs it."
Why not? Because crowded cities and remote areas of poor countries often don't have adequate health facilities nearby; because many parents of young children never learn how to make oral rehydration solution at home; because sachets of the powdered mix require packaging, storage and distribution to those who need them; because oral rehydration does not initially reduce a child's stool output, leading some parents to conclude that it doesn't work, and give up. Because — perhaps above all — our sense of global health priorities is uncomfortably skewed. While diarrhea is a major killer in developing countries, in the rich world it is usually no more than an irritant. So developed nations channel health-care funds into areas perceived as presenting greater risks. Antiviral drugs are purchased and vaccines are ordered to guard against the potential threat from avian influenza instead of getting packages of rehydration solution costing just 6 cent a liter to those at risk of dying from diarrhea elsewhere. But far more children die from diarrhea every day than have ever died from avian flu.
Diseases that have high profiles and vocal activists — such as aids, tuberculosis and malaria — attract far more interest and money from big donors and governments, based partly on the mistaken belief that they kill the most children. Celebrities don't host concerts to fight diarrhea. Of 29 child-health specialists at major international development agencies surveyed by the Rotavirus Vaccine Program — a charity based in Seattle, Washington — 40% named aids, tuberculosis and malaria as the three greatest childhood killers. In reality, the top three are pneumonia, diarrhea and malaria. "This problem isn't getting the attention it deserves," says Wandee Varavithya, a doctor who has treated diarrheal diseases for nearly 40 years in Thailand. That needs to change.
Most cases of diarrhea can be traced to food or water tainted by 100 or so intestinal bugs, most commonly rotavirus, E. coli, shigella, campylobacter and salmonella. Thumb sucking doesn't help; it can lead to what doctors call fecal-oral contamination. "Toddlers will always pick up things and put them into their mouths and, if you don't have a clean environment, that can lead to diarrhea," says Therese Dooley, until recently a unicef project officer in Ethiopia. Infection triggers a cascade of events that can cause diarrhea, if left untreated, to escalate from an unpleasant experience to a life-threatening condition. Normally, 50-75% of the human body is water. The small intestine serves as its key pumping station, absorbing water and nutrients through its walls. There, nutrient-rich fluids enter the bloodstream, which transports them to other parts of the body. But when the intestine detects a pathogen in its midst, it stops soaking up fluids and disgorges its contents in a watery rush of stools. The consequence is what we know as dehydration.
Oral rehydration treatment can reverse dehydration in more than 90% of patients, even in cases of the severe diarrhea caused by bugs like rotavirus and cholera. When the solution reaches the small intestine, the sugar is moved from the hollow part of the intestine into its mucosal lining through the villi, small fingerlike projections on the intestinal wall. "It's like having a chemical needle in the intestinal tract," says William Greenough, a professor of medicine at Johns Hopkins School of Medicine in Baltimore, Maryland, and a former director of ICDDR. Sugar's chemical properties allow salt to be absorbed more efficiently. The salt then promotes the absorption of water into the capillaries within the intestinal wall, which carry the water and electrolytes to other parts of the body and restore fluid balance.
The connection between diarrhea and fluid loss was first noted in 1830 by a surgeon working for the British East India Company in Calcutta. But interest in treating diarrhea didn't gain ground until devastating cholera epidemics swept the subcontinent in the middle of the last century. Fluid loss from cholera-related diarrhea occurs so rapidly that its victims can die within four to eight hours or, as lore has it, before they can dig their own graves. Cholera is still a leading cause of diarrhea in Bangladesh's southern Ganges River basin. Vaccines preventing cholera have never been completely effective or long-lasting, so when ICDDR was established as the Cholera Research Laboratory in 1960, its mission was to evaluate such treatments. By the late 1960s, the facility had begun experimenting with oral rehydration and, within a few years, fatalities among its diarrhea patients had dropped from 50% to zero. Across the Bangladeshi delta, oral rehydration was also gaining ground at the Johns Hopkins Center for Medical Research and Training in Calcutta. Teams at both centers knew they had an effective treatment — but they faced resistance from a profession that dismissed such a basic remedy as inferior to costlier IV saline fluids.
The opportunity to prove oral rehydration's worth came in the form of a disaster. When Bangladesh's war for independence from Pakistan broke out in 1971, 9 million refugees poured into India, bringing cholera with them. Dilip Mahalanabis, an Indian doctor who had participated in the oral rehydration trials at the Johns Hopkins Center in Calcutta, began using IV saline treatment at a border camp, but within weeks his supplies were exhausted. Amid awful scenes in which people walked for days only to die, Mahalanabis and his team drew on their experiences in Calcutta. They formed an assembly line to weigh out correct proportions of rehydration ingredients in plastic bags, sealed the bags with an iron, and mixed the powder with water so patients' friends and relatives could collect it in mugs. "We converted the library at Johns Hopkins into a factory," Mahalanabis, now 79, recalls. "We brought in drums with side-taps, filled them up and sent them to the field. We were essentially using people to experiment on. But we were pushed to the wall. We had no choice." Using lay people to administer the treatment while health workers replenished supplies was controversial. Doctors had long assumed that, in untrained hands, rehydration solution might be prepared in the wrong concentration and kill more patients than it saved.
At the Gafft Primary School, amid the eucalyptus trees of Adet, up to 40% of the students used to suffer regular diarrhea attacks, especially after the rainy season when sewage seeps into water supplies. "If the students get sick," says teacher Tesfaye Birhanu, "they can't learn their lessons and think freely." Until recently, the four toilets shared by Gafft's 1,266 pupils were filthy, and girls like Genet Solomon avoided using them. "Before, I would get sick once a month," says Solomon, 12. Then the school built three simple pit latrines in cinder-block cubicles. A sanitation club began encouraging students to wash their hands after using the toilet and before meals, a simple way of reducing the risk of diarrheal illnesses. Now, fewer than 20% of the students fall ill. Solomon has been sick once in the past six months. "Hand washing is such a simple thing, but it can have a major impact on a child's health," says Unicef's Dooley.
Simple remedies such as oral rehydration and pit latrines don't make the world's headlines. Yet recurrent bouts of diarrhea not only disrupt a child's schooling, but also retard physical development as vital nutrients are continually flushed out of the body. One ray of hope: preliminary studies suggest that zinc supplements protect the intestine's lining and significantly reduce the duration of diarrhea episodes as well as the risk of recurrence. At ICDDR's field research center southeast of Dhaka, children who were given a 10-day course of zinc tablets after developing diarrhea had 30% fewer relapses, and 20% fewer developed pneumonia, reducing overall deaths by 50%. The cost of a course of zinc: about 25�. With funding from the Bill and Melinda Gates Foundation and support from the U.S. Agency for International Development, an ICDDR program now aims to provide zinc tablets to every child under 5 in Bangladesh.
Vaccines also hold promise for preventing some types of diarrhea. The most common cause of diarrhea in children is rotavirus, which leads to severe, watery diarrhea. Researchers believe it infects almost every child in the world by age 5 and kills 600,000 of them a year in poor countries. (Children who contract the virus in rich countries, by contrast, usually recover quickly because they are treated aggressively.) The first vaccine approved for prevention of rotavirus, Wyeth's Rotashield, was taken off the market in 1999 after several children who received it developed a rare but serious complication in which the bowel folds in on itself. Preliminary studies suggest this problem has been overcome by Merck's RotaTeq, which was approved by regulators in Europe and the U.S. earlier this year, and GlaxoSmith-Kline's Rotarix, approved in Europe in February. Like other vaccines, they work by provoking the development of antibodies that protect against future infection. Both are given orally. Clinical trials of both drugs have been encouraging. Evan Simpson, a public-health specialist at the Seattle-based Rotavirus Vaccine Program, says the new vaccines have the potential to reduce deaths from rotavirus-related diarrhea to 200,000 a year. As with oral rehydration treatment and zinc supplements, though, distribution remains a hurdle. "The rotavirus vaccine is a potential silver bullet," Simpson says, "but you've still got to get it to them."
The cost of a vaccine — about $60 a dose in countries such as Canada, France and South Korea — makes distribution difficult in poor parts of the world. Beatrice De Vos, Glaxo's director of worldwide medical affairs, says her company has adopted a "south first" strategy of pricing to provide steep discounts on Rotarix for poorer countries if they have a system for vaccinating all young children. Diarrheal disease experts say Glaxo is selling its vaccine for as little as $7 a dose in Brazil. "For the poorest developing countries that's still unaffordable, but with greater use and greater manufacturing, that price will go down," says Roger I. Glass, director of the U.S. National Institutes of Health's Fogarty International Center and former chief of the viral gastroenteritis unit at the cdc in Atlanta, Georgia.
One dollar is about the price that Thai doctor Wandee would like to pay for the rotavirus vaccine. Rotavirus is the leading cause of diarrhea in Thai children today. In the 40 years since Wandee began championing oral rehydration at the Ramathibodi Hospital in Bangkok, deaths from diarrhea have dropped to 1 in 10,000 diarrhea patients from 1 in 1,000, she says. Thailand has followed a cost-effective approach by organizing education and training workshops on oral rehydration for pediatricians, hospital staff, pharmacists and — most importantly — health workers and volunteers in tiny, remote villages. The country has also developed a system to track outbreaks so that doctors and scientists can work to prevent repeats. That's in contrast to most of Africa and to neighboring Burma, Cambodia and Laos, which Wandee says resist public counts of diarrhea cases lest they put off foreign investors and tourists. "If the governments do their job and allow ngos to reach down to the community level," Wandee says, "we could save more people. We could prevent 2 million deaths a year if we could reach out to all the villages."
Saving 2 million lives a year, you might think, is a cause with which politicians and movie stars would fall over themselves to be associated. But tackling diarrhea has never had the high profile of other public-health crises. There's much to do; though experts know what interventions can reduce needless deaths, getting them in place is not always easy. There are thousands of villages in places such as Bangladesh's muddy delta and the dry northern expanses of Ethiopia that still lack the infrastructure, education and methods of treatment that would protect their children's lives. To be sure, there is some good news; a recent report by unicef found that global access to safe drinking water rose from 1990 to 2004. But 1.1 billion people still don't have clean water; 2.6 billion lack a basic toilet. "That's an infrastructure problem and a development problem that we have not been able to deal with," says Greenough of Johns Hopkins. If the world wants to avoid the needless deaths of yet more children, it's time that we did.
ICDDR spends $20 million a year treating up to 150,000 patients, its budget financed mostly by grants from the government, international aid agencies and charities. At an average cost of $5 a day for each patient, the center stretches that money a long way. When the monsoon season begins, the hospital erects giant tents in its parking lot to cope with the extra patients. But the success of the hospital in Dhaka has not been replicated elsewhere.
In Africa, the fight against diarrhea is hampered by the lack of clean water and the infrastructure necessary to ensure public health. In countries like Ethiopia, only 40% of people have access to safe water, and fewer than 1 in 3 has regular access to safe sanitation, which at a minimum means a pit latrine. Most Ethiopians don't make the connection between the way they dispose of human waste and their family's health; instead, they believe that "diseases are transmitted by the will of God," says Worku Fentahun, head of health for the Banja district in the country's north. As a consequence, the average Ethiopian child suffers five to 12 episodes of diarrhea a year. Based on studies by the country's government and the World Bank, and by the Ethiopian Ministry of Health, between 50,000 and 112,000 Ethiopian children under 5 die from diarrhea every year. So for the past three years, unicef, the government, churches and ngos have led a campaign to teach Ethiopians the basic principles of hygiene, the importance of washing their hands and how to build their own toilets. The government has also trained health extension workers, mostly women, who can then teach other villagers about sanitation.
Cheap; but nothing like as commonly available as it should be. Oral rehydration has saved the lives of more than 40 million children since it was first put to the test during a cholera outbreak among refugees on India's border with Bangladesh in 1971. But decades later, it remains grossly underused. The result, according to the World Health Organization (WHO): 3 million people a year still die from diarrheal complications, including 1.9 million children under 5, or 17% of the estimated 11 million deaths in that age group. These deaths are largely preventable and unnecessary. "We have the tools to really reduce deaths," says Olivier Fontaine, a diarrheal disease expert at the WHO in Geneva, Switzerland. "The cost of this intervention is minimal. Yet we can't get it to every child that needs it."
Why not? Because crowded cities and remote areas of poor countries often don't have adequate health facilities nearby; because many parents of young children never learn how to make oral rehydration solution at home; because sachets of the powdered mix require packaging, storage and distribution to those who need them; because oral rehydration does not initially reduce a child's stool output, leading some parents to conclude that it doesn't work, and give up. Because — perhaps above all — our sense of global health priorities is uncomfortably skewed. While diarrhea is a major killer in developing countries, in the rich world it is usually no more than an irritant. So developed nations channel health-care funds into areas perceived as presenting greater risks. Antiviral drugs are purchased and vaccines are ordered to guard against the potential threat from avian influenza instead of getting packages of rehydration solution costing just 6 cent a liter to those at risk of dying from diarrhea elsewhere. But far more children die from diarrhea every day than have ever died from avian flu.
Diseases that have high profiles and vocal activists — such as aids, tuberculosis and malaria — attract far more interest and money from big donors and governments, based partly on the mistaken belief that they kill the most children. Celebrities don't host concerts to fight diarrhea. Of 29 child-health specialists at major international development agencies surveyed by the Rotavirus Vaccine Program — a charity based in Seattle, Washington — 40% named aids, tuberculosis and malaria as the three greatest childhood killers. In reality, the top three are pneumonia, diarrhea and malaria. "This problem isn't getting the attention it deserves," says Wandee Varavithya, a doctor who has treated diarrheal diseases for nearly 40 years in Thailand. That needs to change.
Most cases of diarrhea can be traced to food or water tainted by 100 or so intestinal bugs, most commonly rotavirus, E. coli, shigella, campylobacter and salmonella. Thumb sucking doesn't help; it can lead to what doctors call fecal-oral contamination. "Toddlers will always pick up things and put them into their mouths and, if you don't have a clean environment, that can lead to diarrhea," says Therese Dooley, until recently a unicef project officer in Ethiopia. Infection triggers a cascade of events that can cause diarrhea, if left untreated, to escalate from an unpleasant experience to a life-threatening condition. Normally, 50-75% of the human body is water. The small intestine serves as its key pumping station, absorbing water and nutrients through its walls. There, nutrient-rich fluids enter the bloodstream, which transports them to other parts of the body. But when the intestine detects a pathogen in its midst, it stops soaking up fluids and disgorges its contents in a watery rush of stools. The consequence is what we know as dehydration.
Oral rehydration treatment can reverse dehydration in more than 90% of patients, even in cases of the severe diarrhea caused by bugs like rotavirus and cholera. When the solution reaches the small intestine, the sugar is moved from the hollow part of the intestine into its mucosal lining through the villi, small fingerlike projections on the intestinal wall. "It's like having a chemical needle in the intestinal tract," says William Greenough, a professor of medicine at Johns Hopkins School of Medicine in Baltimore, Maryland, and a former director of ICDDR. Sugar's chemical properties allow salt to be absorbed more efficiently. The salt then promotes the absorption of water into the capillaries within the intestinal wall, which carry the water and electrolytes to other parts of the body and restore fluid balance.
The connection between diarrhea and fluid loss was first noted in 1830 by a surgeon working for the British East India Company in Calcutta. But interest in treating diarrhea didn't gain ground until devastating cholera epidemics swept the subcontinent in the middle of the last century. Fluid loss from cholera-related diarrhea occurs so rapidly that its victims can die within four to eight hours or, as lore has it, before they can dig their own graves. Cholera is still a leading cause of diarrhea in Bangladesh's southern Ganges River basin. Vaccines preventing cholera have never been completely effective or long-lasting, so when ICDDR was established as the Cholera Research Laboratory in 1960, its mission was to evaluate such treatments. By the late 1960s, the facility had begun experimenting with oral rehydration and, within a few years, fatalities among its diarrhea patients had dropped from 50% to zero. Across the Bangladeshi delta, oral rehydration was also gaining ground at the Johns Hopkins Center for Medical Research and Training in Calcutta. Teams at both centers knew they had an effective treatment — but they faced resistance from a profession that dismissed such a basic remedy as inferior to costlier IV saline fluids.
The opportunity to prove oral rehydration's worth came in the form of a disaster. When Bangladesh's war for independence from Pakistan broke out in 1971, 9 million refugees poured into India, bringing cholera with them. Dilip Mahalanabis, an Indian doctor who had participated in the oral rehydration trials at the Johns Hopkins Center in Calcutta, began using IV saline treatment at a border camp, but within weeks his supplies were exhausted. Amid awful scenes in which people walked for days only to die, Mahalanabis and his team drew on their experiences in Calcutta. They formed an assembly line to weigh out correct proportions of rehydration ingredients in plastic bags, sealed the bags with an iron, and mixed the powder with water so patients' friends and relatives could collect it in mugs. "We converted the library at Johns Hopkins into a factory," Mahalanabis, now 79, recalls. "We brought in drums with side-taps, filled them up and sent them to the field. We were essentially using people to experiment on. But we were pushed to the wall. We had no choice." Using lay people to administer the treatment while health workers replenished supplies was controversial. Doctors had long assumed that, in untrained hands, rehydration solution might be prepared in the wrong concentration and kill more patients than it saved.
- Mahalanabis' gamble paid off. The fatality rate among the patients in the camp fell to 3% from 30%, and to less than 1% when IV fluids were administered to the most severely ill. Still, skepticism about the effectiveness of oral rehydration continued. Several journals refused to publish Mahalanabis' paper about the outbreak. But Dhiman Barua, then head of WHO's bacterial diseases unit in Geneva, Switzerland and a survivor of the massive 1932 cholera epidemic in Bangladesh's southern port city of Chittagong, had visited Mahalanabis' camp. He was converted and pushed oral rehydration through all the U.N. health agencies. who rolled out its diarrheal-diseases control program in 1978. "The simplicity and power of this tool gave it its own momentum," Mahalanabis says. Power indeed: the initiative cut total worldwide diarrhea deaths from about 5 million in 1980 to 3 million today.
In Bangladesh alone, child mortality fell from 35% to 6% over the following 20 years. But far too many people are still dying from preventable diarrheal diseases. Today, according to unicef, diarrhea still claims the lives of 36,000 young Bangladeshi children a year. Infants like Sohag would perish if they didn't live near a hospital — because they were born to parents unfamiliar with oral rehydration. For the third time in 12 days, 6-month-old Ullash has been admitted to the ICDDR's children's ward; just one of 325 patients admitted within the last 24 hours. The boy weighs only 69% of the expected weight for his age and is malnourished. He has a high fever, a cough and persistent diarrhea. His parents, Jurin and Nazdin, educated Dhaka residents, wait anxiously as he receives intravenous fluids. "We don't understand where this is coming from," says Nazdin. But Sack, the center's executive director, knows. Malnutrition and diarrhea go hand-in-hand, and in Bangladesh both are so widespread that not even middle-class children can escape their self-perpetuating cycle. "If you have a child that is malnourished and who then loses more weight through diarrhea, and tries to make it up, but never makes it up because he is weak and has another episode of diarrhea, then it doesn't matter how well-off the parents are," he says. "That is a child who is on the road to death."
At the Gafft Primary School, amid the eucalyptus trees of Adet, up to 40% of the students used to suffer regular diarrhea attacks, especially after the rainy season when sewage seeps into water supplies. "If the students get sick," says teacher Tesfaye Birhanu, "they can't learn their lessons and think freely." Until recently, the four toilets shared by Gafft's 1,266 pupils were filthy, and girls like Genet Solomon avoided using them. "Before, I would get sick once a month," says Solomon, 12. Then the school built three simple pit latrines in cinder-block cubicles. A sanitation club began encouraging students to wash their hands after using the toilet and before meals, a simple way of reducing the risk of diarrheal illnesses. Now, fewer than 20% of the students fall ill. Solomon has been sick once in the past six months. "Hand washing is such a simple thing, but it can have a major impact on a child's health," says Unicef's Dooley.
Simple remedies such as oral rehydration and pit latrines don't make the world's headlines. Yet recurrent bouts of diarrhea not only disrupt a child's schooling, but also retard physical development as vital nutrients are continually flushed out of the body. One ray of hope: preliminary studies suggest that zinc supplements protect the intestine's lining and significantly reduce the duration of diarrhea episodes as well as the risk of recurrence. At ICDDR's field research center southeast of Dhaka, children who were given a 10-day course of zinc tablets after developing diarrhea had 30% fewer relapses, and 20% fewer developed pneumonia, reducing overall deaths by 50%. The cost of a course of zinc: about 25�. With funding from the Bill and Melinda Gates Foundation and support from the U.S. Agency for International Development, an ICDDR program now aims to provide zinc tablets to every child under 5 in Bangladesh.
Vaccines also hold promise for preventing some types of diarrhea. The most common cause of diarrhea in children is rotavirus, which leads to severe, watery diarrhea. Researchers believe it infects almost every child in the world by age 5 and kills 600,000 of them a year in poor countries. (Children who contract the virus in rich countries, by contrast, usually recover quickly because they are treated aggressively.) The first vaccine approved for prevention of rotavirus, Wyeth's Rotashield, was taken off the market in 1999 after several children who received it developed a rare but serious complication in which the bowel folds in on itself. Preliminary studies suggest this problem has been overcome by Merck's RotaTeq, which was approved by regulators in Europe and the U.S. earlier this year, and GlaxoSmith-Kline's Rotarix, approved in Europe in February. Like other vaccines, they work by provoking the development of antibodies that protect against future infection. Both are given orally. Clinical trials of both drugs have been encouraging. Evan Simpson, a public-health specialist at the Seattle-based Rotavirus Vaccine Program, says the new vaccines have the potential to reduce deaths from rotavirus-related diarrhea to 200,000 a year. As with oral rehydration treatment and zinc supplements, though, distribution remains a hurdle. "The rotavirus vaccine is a potential silver bullet," Simpson says, "but you've still got to get it to them."
The cost of a vaccine — about $60 a dose in countries such as Canada, France and South Korea — makes distribution difficult in poor parts of the world. Beatrice De Vos, Glaxo's director of worldwide medical affairs, says her company has adopted a "south first" strategy of pricing to provide steep discounts on Rotarix for poorer countries if they have a system for vaccinating all young children. Diarrheal disease experts say Glaxo is selling its vaccine for as little as $7 a dose in Brazil. "For the poorest developing countries that's still unaffordable, but with greater use and greater manufacturing, that price will go down," says Roger I. Glass, director of the U.S. National Institutes of Health's Fogarty International Center and former chief of the viral gastroenteritis unit at the cdc in Atlanta, Georgia.
One dollar is about the price that Thai doctor Wandee would like to pay for the rotavirus vaccine. Rotavirus is the leading cause of diarrhea in Thai children today. In the 40 years since Wandee began championing oral rehydration at the Ramathibodi Hospital in Bangkok, deaths from diarrhea have dropped to 1 in 10,000 diarrhea patients from 1 in 1,000, she says. Thailand has followed a cost-effective approach by organizing education and training workshops on oral rehydration for pediatricians, hospital staff, pharmacists and — most importantly — health workers and volunteers in tiny, remote villages. The country has also developed a system to track outbreaks so that doctors and scientists can work to prevent repeats. That's in contrast to most of Africa and to neighboring Burma, Cambodia and Laos, which Wandee says resist public counts of diarrhea cases lest they put off foreign investors and tourists. "If the governments do their job and allow ngos to reach down to the community level," Wandee says, "we could save more people. We could prevent 2 million deaths a year if we could reach out to all the villages."
Saving 2 million lives a year, you might think, is a cause with which politicians and movie stars would fall over themselves to be associated. But tackling diarrhea has never had the high profile of other public-health crises. There's much to do; though experts know what interventions can reduce needless deaths, getting them in place is not always easy. There are thousands of villages in places such as Bangladesh's muddy delta and the dry northern expanses of Ethiopia that still lack the infrastructure, education and methods of treatment that would protect their children's lives. To be sure, there is some good news; a recent report by unicef found that global access to safe drinking water rose from 1990 to 2004. But 1.1 billion people still don't have clean water; 2.6 billion lack a basic toilet. "That's an infrastructure problem and a development problem that we have not been able to deal with," says Greenough of Johns Hopkins. If the world wants to avoid the needless deaths of yet more children, it's time that we did.
ICDDR spends $20 million a year treating up to 150,000 patients, its budget financed mostly by grants from the government, international aid agencies and charities. At an average cost of $5 a day for each patient, the center stretches that money a long way. When the monsoon season begins, the hospital erects giant tents in its parking lot to cope with the extra patients. But the success of the hospital in Dhaka has not been replicated elsewhere.
In Africa, the fight against diarrhea is hampered by the lack of clean water and the infrastructure necessary to ensure public health. In countries like Ethiopia, only 40% of people have access to safe water, and fewer than 1 in 3 has regular access to safe sanitation, which at a minimum means a pit latrine. Most Ethiopians don't make the connection between the way they dispose of human waste and their family's health; instead, they believe that "diseases are transmitted by the will of God," says Worku Fentahun, head of health for the Banja district in the country's north. As a consequence, the average Ethiopian child suffers five to 12 episodes of diarrhea a year. Based on studies by the country's government and the World Bank, and by the Ethiopian Ministry of Health, between 50,000 and 112,000 Ethiopian children under 5 die from diarrhea every year. So for the past three years, unicef, the government, churches and ngos have led a campaign to teach Ethiopians the basic principles of hygiene, the importance of washing their hands and how to build their own toilets. The government has also trained health extension workers, mostly women, who can then teach other villagers about sanitation.
"Diarrhea is the world’s most effective weapon of mass destruction."
Children with diarrhoea are at risk of dying due to dehydration, and early and appropriate fluid replacement is a main intervention to prevent death. Yet few children with diarrhoea in developing countries receive appropriate treatment with oral rehydration therapy and continued feeding (39 per cent).
Even fewer receive solutions made of oral rehydration salts (ORS) alone (one-third), and the past decade has seen no real progress in improving coverage across developing countries.
Moreover, the poorest children in the poorest countries are least likely to use ORS, and zinc treatment remains largely unavailable in high-mortality countries. The stagnant low ORS coverage over the past decade indicates a widespread failure to deliver one of the most cost-effective and life-saving child survival interventions and underscores the urgent need to refocus attention and funding on diarrhoea control."
Source: UNICEF - Pneumonia and diarrhoea: Tackling the deadliest diseases for the world’s poorest children
see: rehydration project